Acne is a familiar skin concern that many of us have encountered at some point in our lives. But have you ever wondered what exactly causes those pesky breakouts? Understanding the biological reason behind acne can shed light on effective remedies and prevention methods. In this article, we will explore the underlying factors that contribute to this common skin condition and gain insight into how we can better manage and combat acne. So, whether you’re dealing with occasional blemishes or persistent acne, get ready to uncover the fascinating science behind it all!
1. Overview of Acne
1.1 Definition of Acne
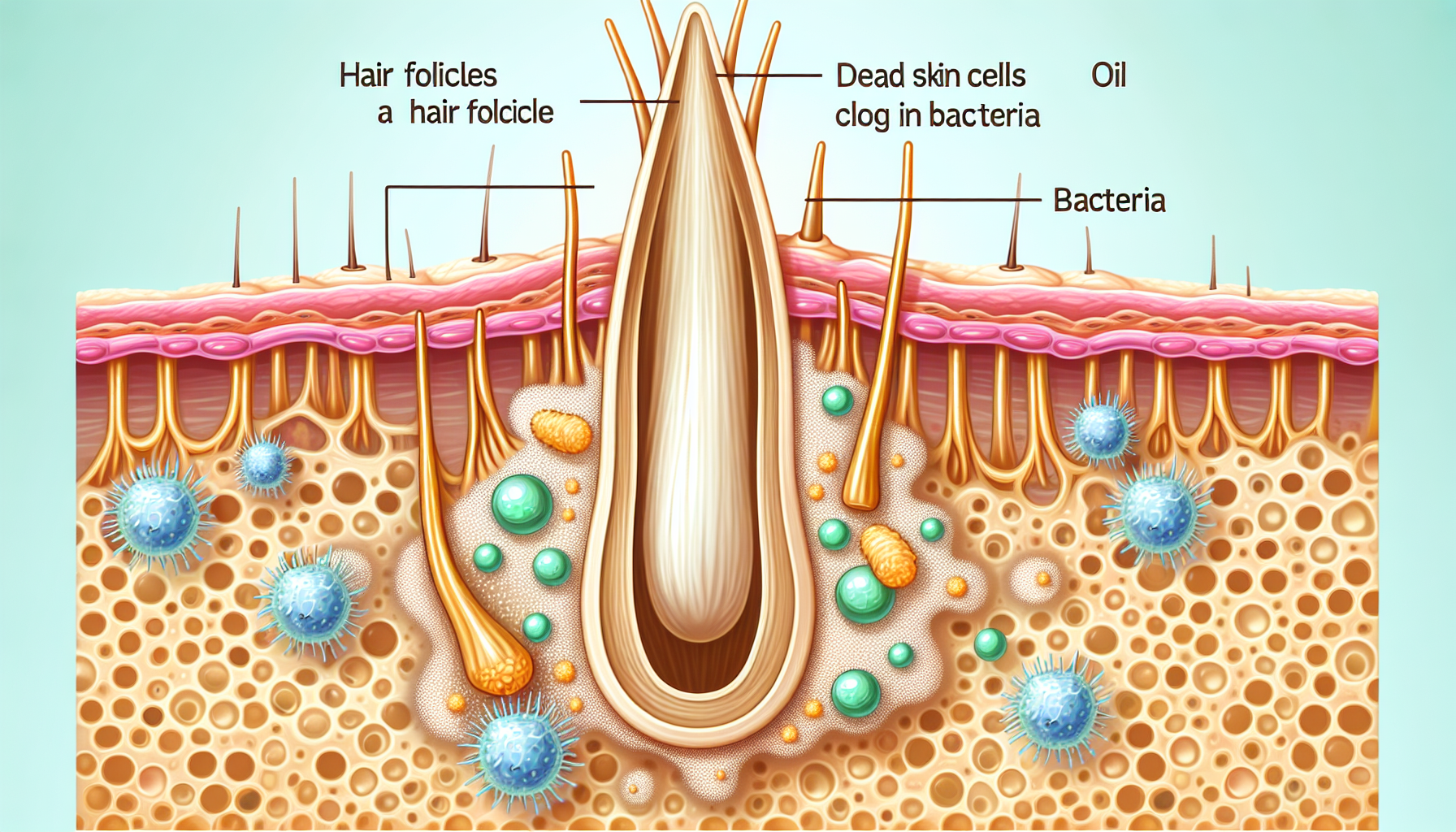
Acne is a common skin condition that occurs when hair follicles become clogged with dead skin cells, oil, and bacteria. It is characterized by the presence of pimples, blackheads, whiteheads, and sometimes, cysts or nodules. Acne can affect people of all ages, but it is most commonly seen during adolescence.
1.2 Prevalence of Acne
Acne is one of the most prevalent skin conditions, affecting millions of people worldwide. It is estimated that about 85% of individuals between the ages of 12 and 24 experience acne at some point. However, acne can persist into adulthood, with approximately 20% of adults over the age of 25 experiencing acne flare-ups.
1.3 Types of Acne
There are different types of acne, each presenting with unique characteristics. The most common type is acne vulgaris, which includes the typical pimples, blackheads, and whiteheads. Other types of acne include cystic acne, which is characterized by painful, inflamed cysts, and nodular acne, which presents as large, hard bumps deep within the skin.
2. Anatomy of the Skin
2.1 Layers of the Skin
The skin is the largest organ of the body and is comprised of three main layers: the epidermis, dermis, and subcutis. The epidermis is the outermost layer, providing a protective barrier against environmental factors. The dermis is located beneath the epidermis and contains blood vessels, nerves, and hair follicles. The subcutis, also known as the hypodermis, is the deepest layer of the skin and is composed of fat tissue.
2.2 Function of the Skin
The skin serves various functions, including protection, regulation, and sensation. It acts as a physical barrier, preventing the entry of harmful substances and pathogens. The skin also plays a role in regulating body temperature by controlling sweat production and blood flow. Additionally, the skin contains sensory receptors that allow us to perceive touch, temperature, and pain.
2.3 Sebaceous Glands
Sebaceous glands are small, oil-producing glands that are present throughout the skin, with higher concentrations found on the face, chest, and back. These glands are connected to hair follicles and produce a substance called sebum. Sebum plays a crucial role in keeping the skin moisturized and protected.
3. Understanding Acne Vulgaris
3.1 What is Acne Vulgaris?
Acne vulgaris, the most common form of acne, is characterized by the formation of comedones (blackheads and whiteheads), papules, pustules, and sometimes, cysts or nodules. It typically occurs during adolescence due to hormonal changes, but can also affect adults. Acne vulgaris is influenced by several factors, including hormonal imbalances, sebum production, follicular hyperkeratinization, bacterial involvement, inflammation, genetic predisposition, and environmental influences.
3.2 Factors Influencing Acne Vulgaris
Several factors play a role in the development and progression of acne vulgaris. Hormonal changes, particularly during puberty, can trigger increased sebum production, leading to clogged pores. Genetic factors also contribute to an individual’s predisposition to developing acne. Additionally, environmental factors such as diet and stress can exacerbate acne symptoms.
3.3 Pathogenesis of Acne Vulgaris
The pathogenesis of acne vulgaris involves multiple interconnected factors. It begins with the overproduction of sebum by the sebaceous glands, which leads to the accumulation of oil within the hair follicles. This excess sebum, combined with dead skin cells, blocks the follicles, creating an ideal environment for the proliferation of bacteria, particularly Propionibacterium acnes. The presence of bacteria triggers an inflammatory response, leading to the formation of inflammatory acne lesions such as papules and pustules.
4. Role of Hormones
4.1 Hormonal Changes in Puberty
Puberty is a period of significant hormonal changes, particularly the activation of the reproductive system. During this time, the levels of hormones such as androgens, including testosterone, increase. Androgens play a crucial role in the development of primary and secondary sexual characteristics, but they also have an impact on sebum production.
4.2 Androgens and Sebum Production
Androgens stimulate the sebaceous glands to produce sebum. Sebum is necessary for maintaining the skin’s moisture levels, but an excess of sebum can lead to clogged pores. Androgens also influence the differentiation of skin cells, leading to an increased shedding of cells within the hair follicles.
4.3 Impact of Hormones on Acne
The hormonal changes that occur during puberty and throughout the menstrual cycle can contribute to the development of acne. The increased production of sebum under the influence of androgens, combined with the shedding of skin cells and the proliferation of bacteria, creates an environment conducive to the formation of acne lesions.
5. Sebum Production and Acne
5.1 Sebaceous Glands and Sebum
Sebaceous glands are responsible for the production of sebum, an oily substance that lubricates and protects the skin. These glands are most concentrated in areas where acne commonly occurs, such as the face, chest, and back. Sebum contains lipids, cholesterol, and fatty acids, which help maintain the integrity of the skin barrier.
5.2 Relationship Between Sebum and Acne
While sebum is necessary for healthy skin, excessive sebum production can contribute to acne development. When sebum production is increased, the excess oil combines with dead skin cells, bacteria, and other debris, leading to the formation of comedones and the subsequent inflammation associated with acne.
5.3 Effect of Excess Sebum on the Skin
Excess sebum can result in the clogging of hair follicles, leading to the formation of comedones. These comedones can become inflamed and infected, resulting in the formation of papules, pustules, and other acne lesions. Additionally, the presence of excess sebum on the skin’s surface can create an oily appearance and contribute to the development of shiny, greasy skin.
6. Follicular Hyperkeratinization
6.1 Definition of Hyperkeratinization
Follicular hyperkeratinization refers to the abnormal accumulation of dead skin cells within the hair follicles. Normally, the skin cells shed naturally, but in cases of hyperkeratinization, they stick together and become trapped within the follicles, contributing to the development of acne.
6.2 Role of Follicular Hyperkeratinization
Follicular hyperkeratinization is a key factor in the pathogenesis of acne. When dead skin cells become trapped within the follicles, they mix with sebum and other debris, forming a plug that blocks the follicle. This blockage prevents the normal flow of sebum, leading to its accumulation and the subsequent development of acne lesions.
6.3 Connection with Acne Formation
The accumulation of dead skin cells due to follicular hyperkeratinization creates the ideal environment for the growth of bacteria, such as Propionibacterium acnes. This bacterial overgrowth can trigger an inflammatory response in the skin, resulting in the formation of acne lesions.
7. Bacterial Involvement: Propionibacterium acnes
7.1 Overview of Propionibacterium acnes
Propionibacterium acnes is a type of bacteria that resides on the skin’s surface. While it is a normal part of the skin’s microbiota, an overgrowth of this bacterium can contribute to the development of acne. P. acnes produces substances that can trigger inflammation and contribute to the formation of acne lesions.
7.2 Role of Bacteria in Acne
Bacterial involvement is an important aspect of acne development. P. acnes thrives in the clogged hair follicles, where it feeds on the accumulated sebum. This bacterial growth triggers an immune response, leading to inflammation and the characteristic redness and swelling associated with acne.
7.3 Inflammation and Acne
The presence of bacteria within the clogged hair follicles stimulates the release of inflammatory mediators by the immune system. These mediators, including cytokines and chemokines, lead to the dilation of blood vessels and increased blood flow to the affected area. Inflammatory cells, such as neutrophils and macrophages, are recruited to the site, resulting in the formation of papules, pustules, and other inflammatory acne lesions.
8. Impact of Inflammation
8.1 Inflammatory Response
Inflammation is a complex biological response triggered by the body’s immune system to protect against harmful stimuli, such as infections or injuries. It involves the release of biochemical mediators, migration of immune cells, and increased blood flow to the affected area. While inflammation is a normal and protective response, chronic inflammation can contribute to various conditions, including acne.
8.2 Acne Inflammation
In acne, inflammation occurs as a result of the body’s response to the presence of bacteria and other irritants within the clogged hair follicles. The immune system releases inflammatory mediators that cause redness, swelling, and pain, leading to the formation of inflamed acne lesions.
8.3 Link Between Inflammation and Acne
Inflammation plays a significant role in the development and progression of acne. It not only contributes to the formation of inflammatory acne lesions but also prolongs the healing process and increases the risk of scarring. Additionally, chronic inflammation may further disrupt the delicate balance of the skin, leading to a cycle of acne flares.
9. Genetic Factors
9.1 Hereditary Influence on Acne
Genetic factors play a role in an individual’s predisposition to developing acne. Studies have shown that individuals with a family history of acne are more likely to develop the condition themselves. Genetic factors influence various aspects of acne, including sebum production, follicular hyperkeratinization, and the inflammatory response.
9.2 Acne-Related Genes
Several genes have been identified as potentially contributing to acne susceptibility. These genes are involved in processes such as sebum production, inflammation, and the regulation of skin cell turnover. Variations in these genes can influence an individual’s likelihood of developing acne and the severity of their symptoms.
9.3 Genetic Predisposition to Acne
While genetics play a role in acne development, it is important to note that acne is a complex, multifactorial condition. Genetic predisposition alone is not sufficient to cause acne. Environmental factors, hormonal changes, and other influences also contribute to the development and progression of acne.
10. Environmental Factors
10.1 Impact of Environmental Factors
Environmental factors can contribute to acne development by influencing factors such as sebum production, skin cell turnover, and inflammation. Some common environmental factors associated with acne include diet, pollution, humidity, and exposure to certain chemicals or cosmetics.
10.2 Diet and Acne
Research suggests that certain dietary factors can influence acne. High glycemic index foods, such as refined carbohydrates and sugar, may trigger hormonal changes that increase sebum production and inflammation. Additionally, diets high in dairy products and foods containing high levels of saturated fats may exacerbate acne symptoms.
10.3 Stress and Acne
Stress can have a significant impact on acne. When the body is under stress, it releases stress hormones, such as cortisol, which can increase sebum production and inflammation. Stress can also disrupt the balance of the skin’s microbiota and impair the natural healing process, making acne symptoms worse.
In conclusion, acne is a multifactorial skin condition influenced by hormonal changes, sebum production, follicular hyperkeratinization, bacterial involvement, inflammation, genetic predisposition, and environmental factors. Understanding the biological mechanisms underlying acne can help inform prevention and treatment strategies. By addressing these factors holistically, incorporating proper skincare routines, maintaining a healthy diet, managing stress, and seeking appropriate medical care, individuals can better manage and reduce the impact of acne on their overall well-being.